Here is a personal example Colossians 158 S– The faith and love that spring from the hope that is stored up for you in heaven and that you have already heard about in the word of truth, the gospel that has come to youAll over the world this gospel is bearing fruit and growing, just as it has been doing among you since the day you heard it and understood God'sWhether covered by insurance or not, good clinical notes support the rationale for treatment and are necessary should there be a lawsuit or medical issue that requires the patient record be examined The following is an explanation in lay terms as toStudents Organized Against Poverty Students Organized Against Prejudice Subject, Occasion, Audience, and Purpose (education) Subjective Objective Action and Plan of treatment (Chiropractic) Summary On A Page Supertanker Operational Assessment
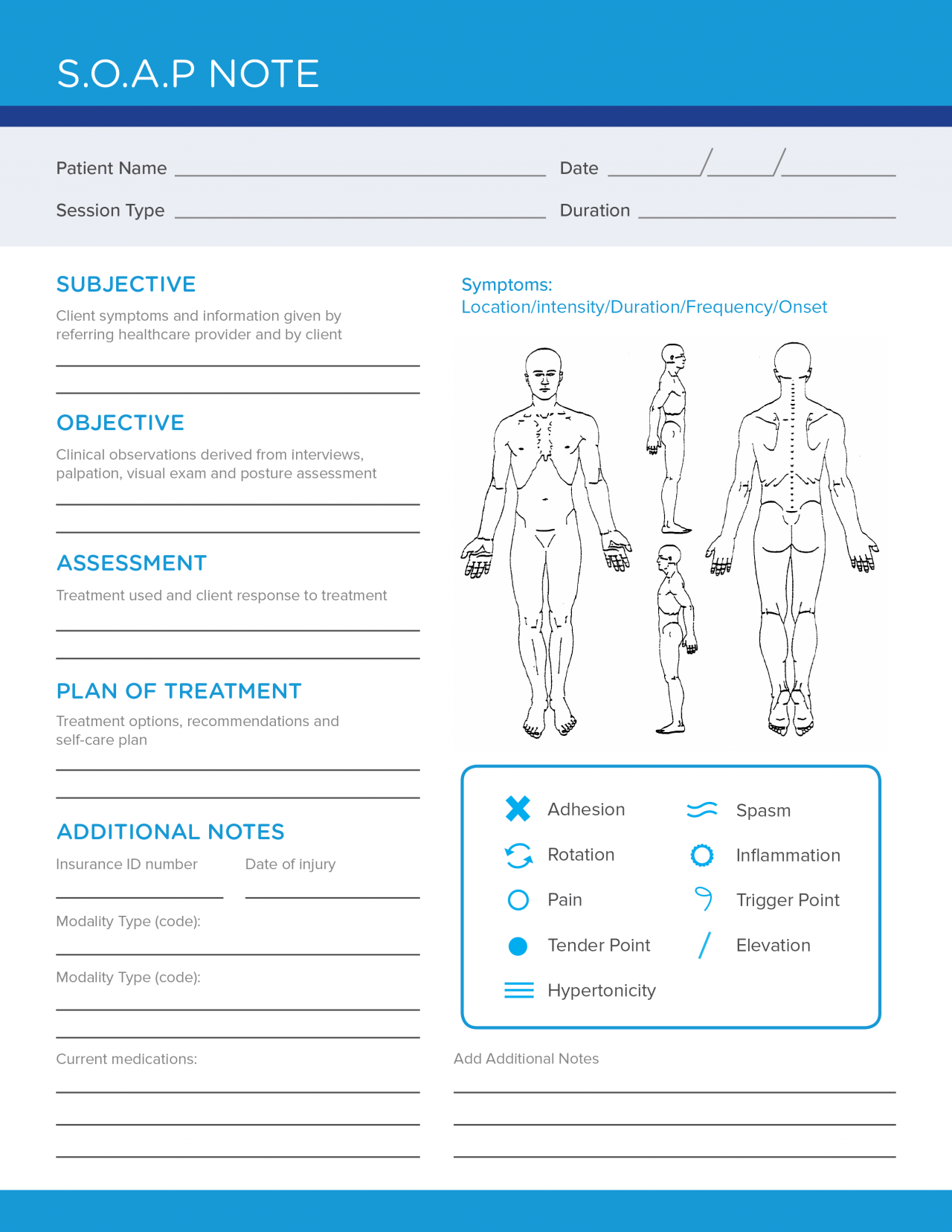
40 Fantastic Soap Note Examples Templates ᐅ Templatelab
S.o.a.p meaning medical
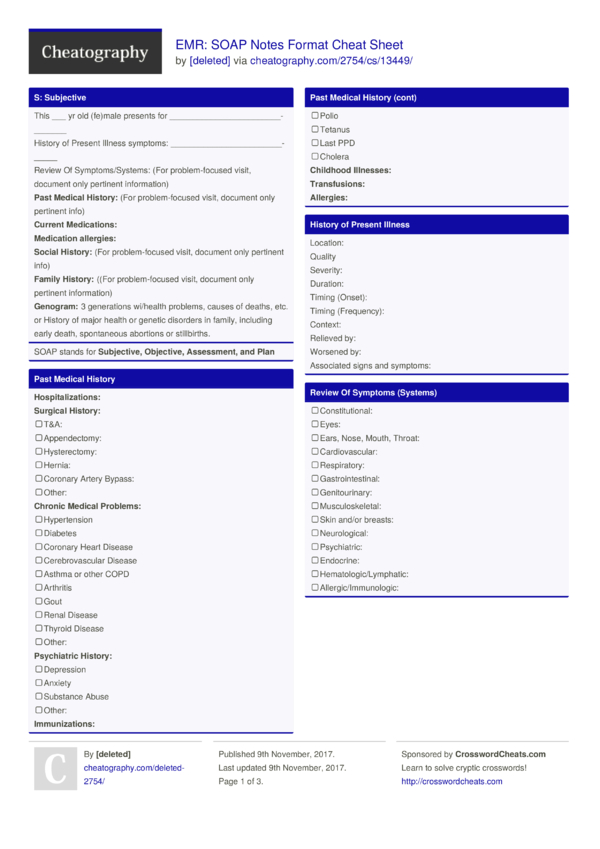
S.o.a.p meaning medical-P The last section is the P, or plan, section In this section, medical professionals plan the course of treatment based on the diagnosis In which part of the SOAP note are the vital signs recorded?Sometimes they simply state in a narrative way the




Hygiene Wikipedia
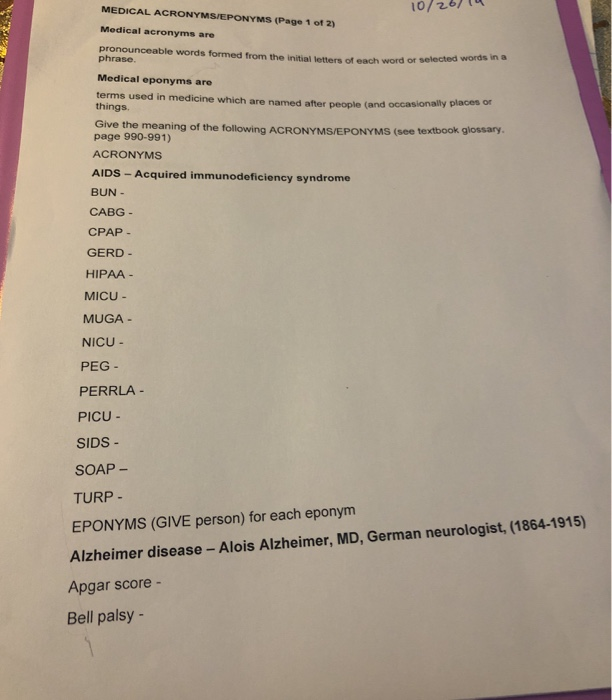
Medical steam piping duct symbols plumbing mechanical / plumbing symbols and abbreviations abbreviations drawing notations sections and details north first floor plan mechanical demolition north crawl space plan mechanical demolition demolition legend demolition plan notesSOAP subjective, objective assessment plan SOB shortness of breath S/P, s/p status post (previous condition) sp cd spinal cord spec specimen sp fl spinal fluid sp&H speech and hearing spin spine, spinal spont spontaneous s/s signs and symptoms SS social service ST speech therapy stat, STAT immediately STD sexually transmitted diseaseUsed in medical records
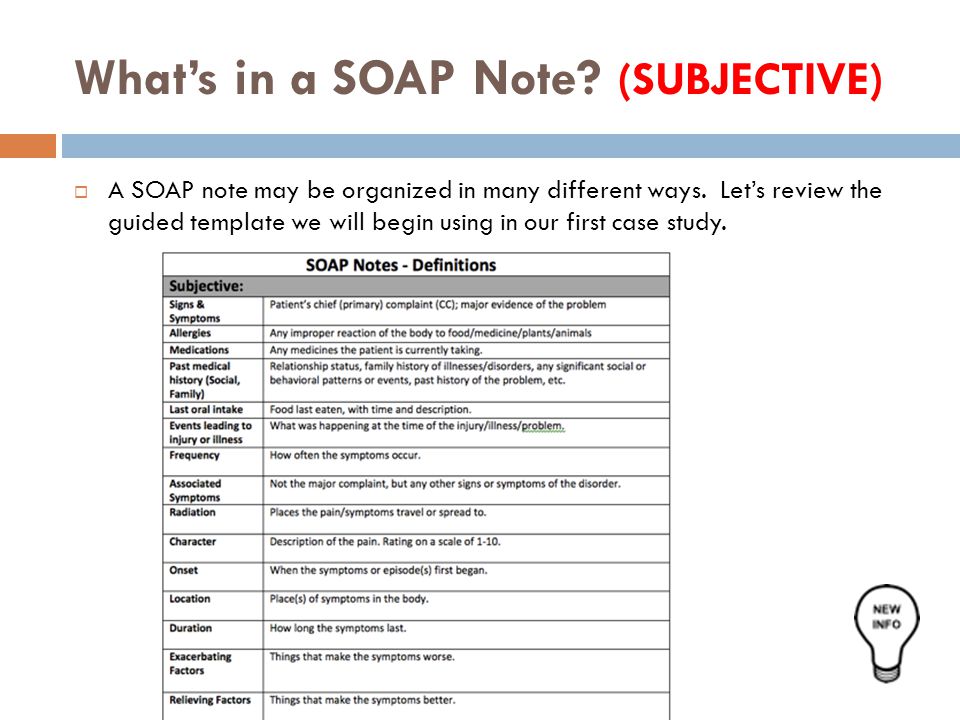
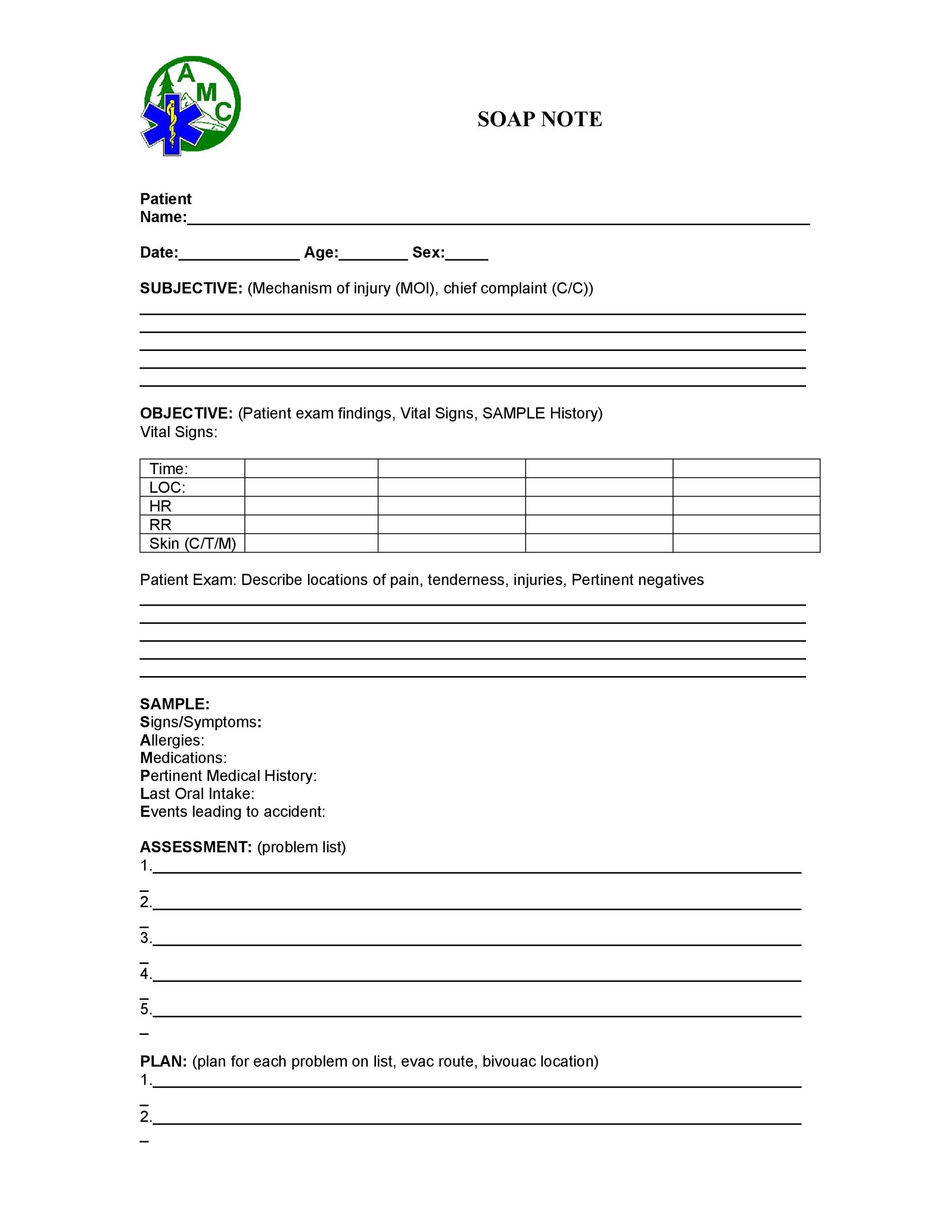
What does the O mean in HOPS Compare the non hurt to the injury, look for bleeding, deformity, swelling,discoloration,scars, and other signs of trauma What does the P mean in HOPSS stands for subjective data provided by the patient, O for objective data gathered by health care professionals in the clinical setting, A for the assessment of the patient's condition, and P for the plan for the patient's care All the slick Web pages, billboards, telephone marketers, direct mailings and open houses cannot compete with the most important clinical tool—SOAP, which stands for Subjective observation, Objective observation, Assessment and Plan A complete individual patient assessment should be performed consistently at every visit How to use SOAP
SOAP is an acronym for Subjective, Objective, Assessment, Plan Search for abbreviation meaning, word to abbreviate, or category Shortcuts for power users examples Abbreviation meaning COB means To abbreviate Management abbreviated Category Medical terms Abbreviation in category Bae in slangAcronym for the conceptual device used by clinicians to organize the progress notes in the problemoriented record;Looking for the definition of EMS?



Www Wto Org English News E News E Rese 03apr E Pdf



Psa Jimmy Caputo Period 5b Storyboard Von
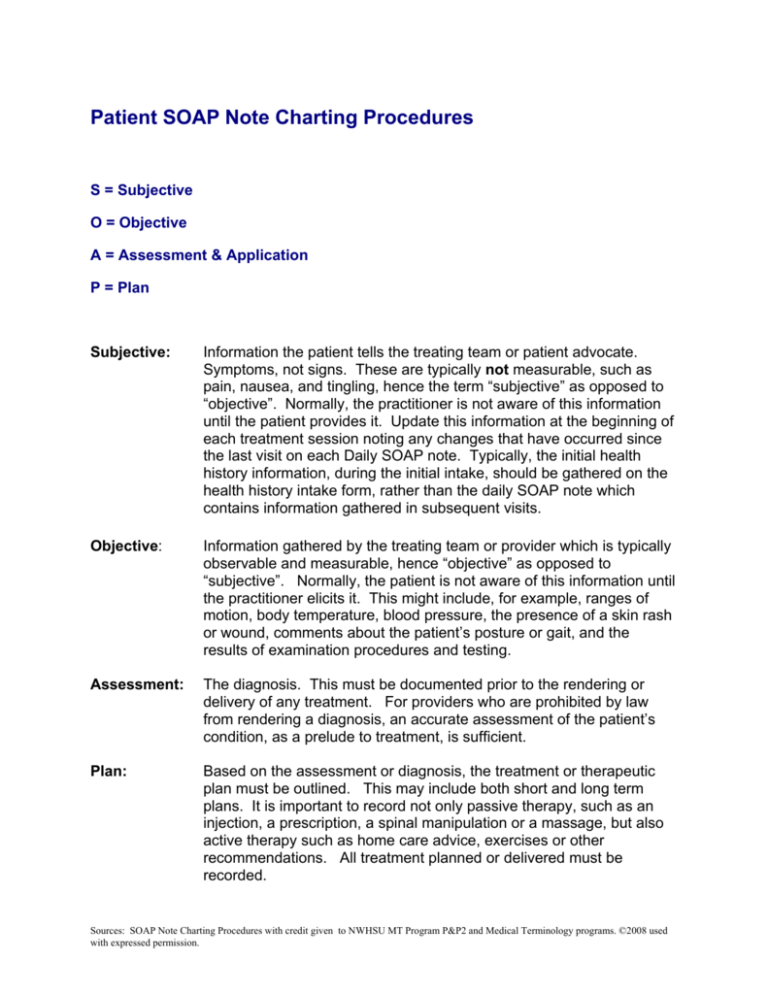
A medical charting system, in which S = Subjective (what the client says, or subjective impressions) O = Objective (what the provider's findings are, or clinical data) A = Assessment (Any changes, the diagnosis, or what the client's condition is) P = Plan for the next treatment, (further studies and suggested treatment)MCH mean corpuscular hemoglobin MCHC mean corpuscular hemoglobin concentration MCV mean corpuscular volume med medical, medid meds medicines 4 mEq/1 milliequivalent per liter Mg milligram MI myocardial infarction (heart attack)R/O abbreviation for rule out;



How To Document A Patient Assessment Soap Geeky Medics




What Is Chlorhexidine Soap With Pictures
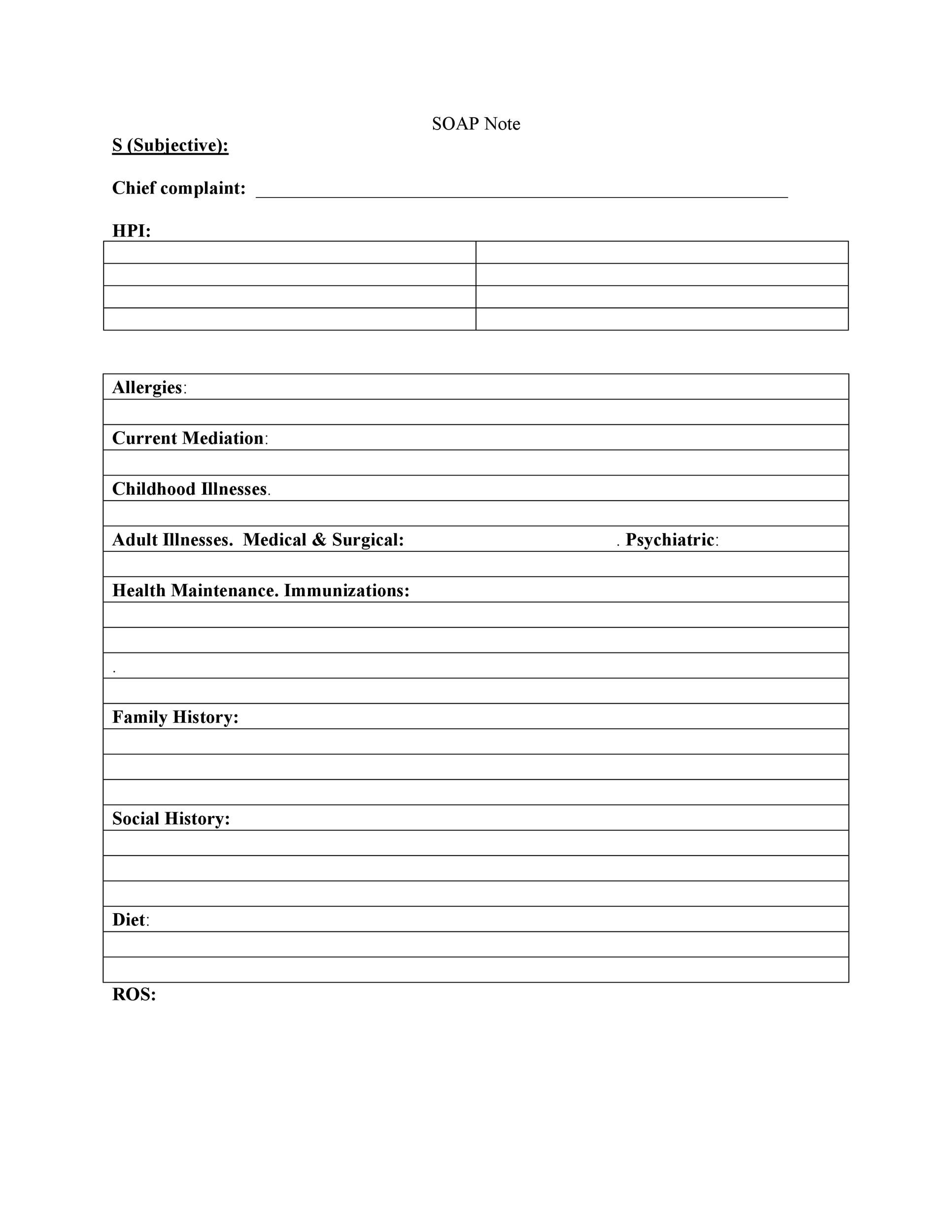
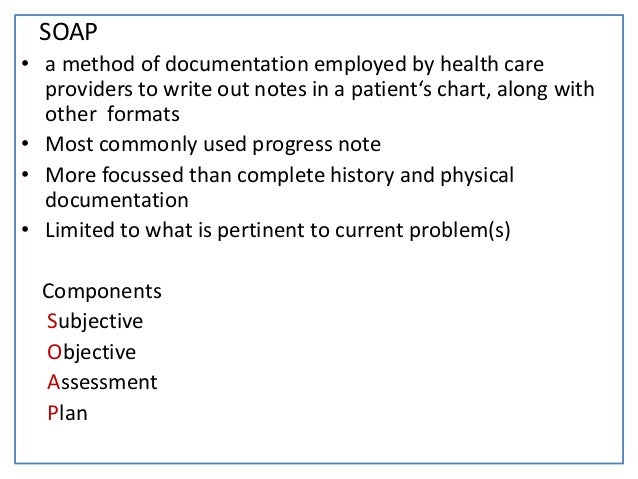
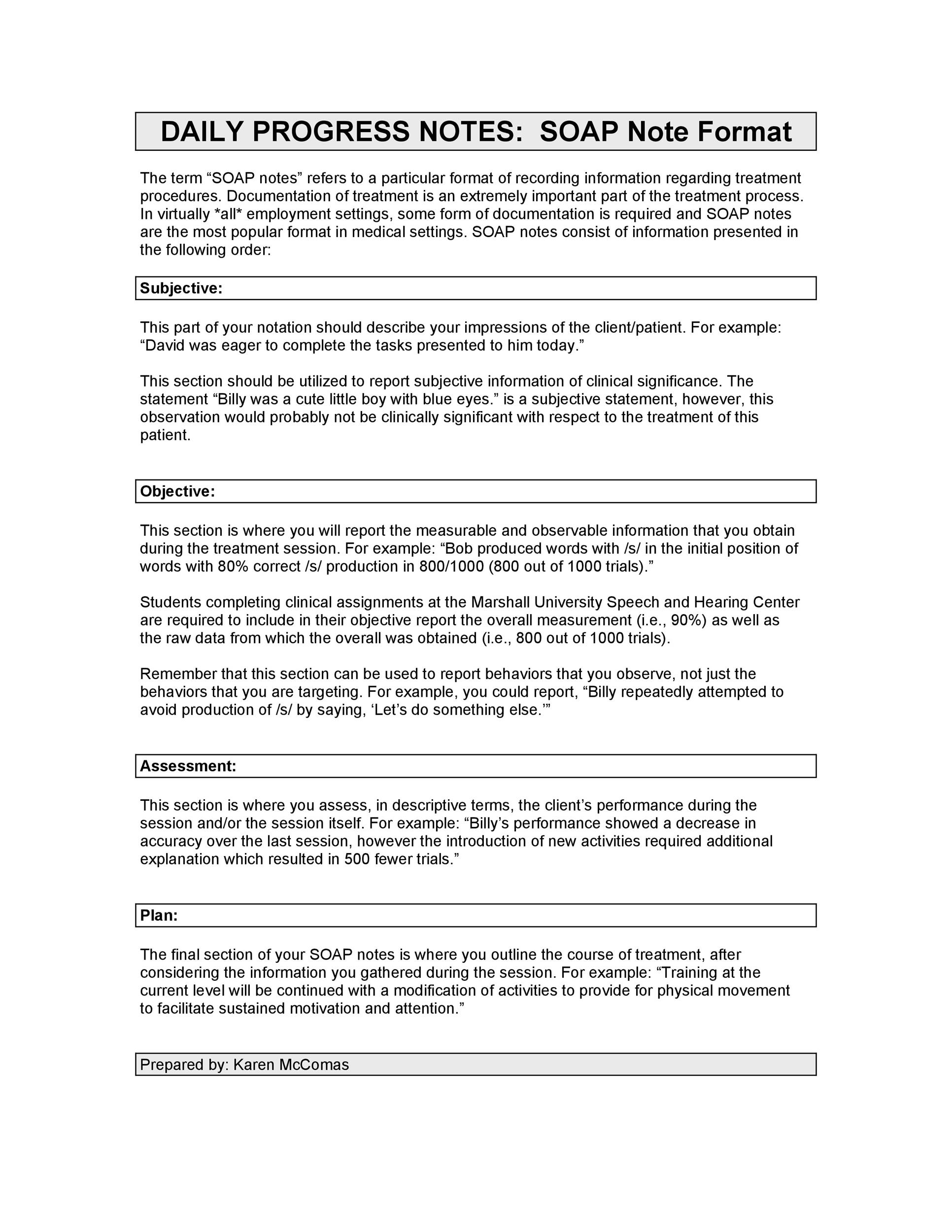
The SOAP note stands for Subjective, Objective, Assessment, and Plan This note is widely used in medical industry Doctors and nurses use SOAP note to document and record the patient's condition and status The SOAP note is considered as the most effective and standard documentation used in the medical industry along with the progress note There are four components that form these notes that make up the acronym SOAP S is for subjective, or what the patients say about their situation It includes a patient's complaints, sensationsSOAPE is listed in the World's largest and most authoritative dictionary database of



Lesson 1 8 The Soap Note Unit 1 Mental Health Ppt Video Online Download



Tips For Writing Better Mental Health Soap Notes Updated 21
Certain medical abbreviations are avoided to prevent mistakes, according to best practices (and in some cases regulatory requirements);Miami Dade College Medical Center Campus Emergency Medical Technician SSOAP OAP RReport eport FFormatormat (S)ubjective In this area you will document anything that the patient or family & friends tell youO In this section, medical




Antibacterial Soap Vs Regular Soap Which One Is Better




Handwriting Text Writing Ask Your Doctor Concept Meaning Seeking Information Or Advice From A Medical Professional Canstock
SOAP Notes in the Medical Field The SOAP note is an essential method of documentation in the medical field It's imperative that every student learn the basics for writing a SOAP note to become a health care provider like a physician or an Advanced Practice NurseThese are flagged in the list of abbreviations used in medical prescriptions Orthographic styling Periods (stops) Periods (stops) are often used in styling abbreviations Prevalent practice in medicine today isBY Matt Soniak iStock A lot of people think that the distress signal is an abbreviation




The Definitive Guide To Ifu For Medical Devices Eu Us
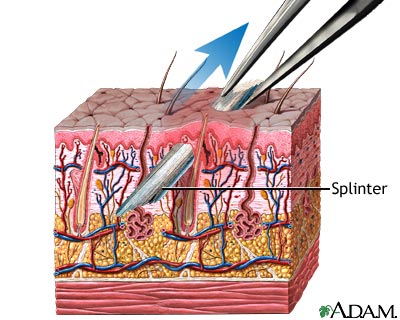



Splinter Removal Medlineplus Medical Encyclopedia
Find out what is the full meaning of EMS on Abbreviationscom! Creating a record of detailed treatment notes allows a medical professional to build their own miniresearch library You will note what works, what doesn't and everything in between Writing great Physical Therapist SOAP notes is a tried and true method for collecting data This data provides reference points throughout a patient's journeySymbolic Optimal Assembly Program (programming language for the IBM 650 computer in the late 1950's) SOAP Spectrometric Oil Analysis Program SOAP Small Operator Assistance Program SOAP Satellite Orbit Analysis Program (standard program




Proper Hand Washing Visual Guide And Tips




What Is A Soap Note Jess Brantner Wvu Dietetic Intern
Looking for online definition of SOAPE or what SOAPE stands for? A SOAP note is information about the patient, which is written or presented in a specific order, which includes certain components SOAP notes are used for admission notes, medical histories and other documents in a patient's chart Call your doctor for medical advice about side effects You may report side effects to FDA at 1800FDA10 FML SOP side effects (more detail) What other drugs will affect FML SOP?



Medical Mnemonics Diagnostic Criteria For Sle Soap Brain Md Usmle Internal Medicine Abim Board Exam Review Blog




Medical Precaution High Resolution Stock Photography And Images Alamy
How do I SOAP?Medical Chart Notes SOAP A chart note usually follows a very simple pattern S ubjective (what the patient thinks) = S O bjective (what the doctor thinks) = O A ssessment (what the diagnosis is) = A P lan (what happens next) = P Not all providers dictate the "SOAP" note format;Medicine used in the eyes is not likely to be affected by other drugs you use But many drugs can interact with each other




Hygiene Wikipedia




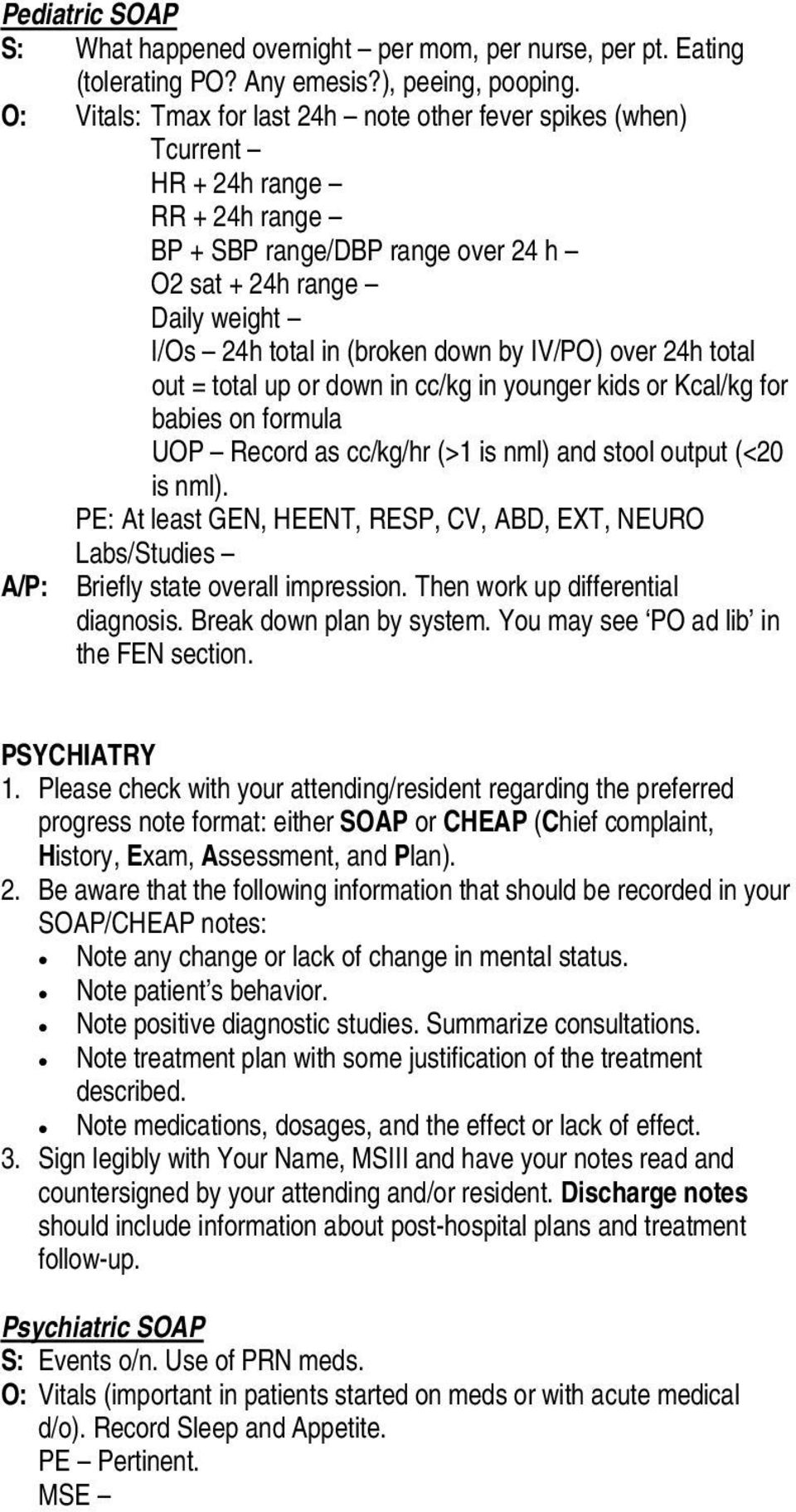
Clerkship Guide Amboss
It's a template for documentation S Subjective a description of the information you received that cannot be proven, specifically measured or independently verified, eg "Nurse I am in pain" O Objective anything that can be measured, observeList of 3 best SOAP meaning forms based on popularity Most common SOAP abbreviation full forms updated in June 21SOAP is listed in the World's largest and most authoritative dictionary database of



51 Sample Soap Notes In Pdf Ms Word Excel



Using Medical Note Taking Skills On Teaching Journal Kwarrior Eng Clinic
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan Each category is described below S = Subjective or symptoms and reflects the history and interval history of the condition The patient's presenting complaints should be described in some detail in the notes of each and every office visitS O A P NOTE S = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session 1 If adding your own explanatory information, place within brackets to make it clear that it is not a direct quote Why SOAP Notes Are an Important Tool SOAP is the most common format used by medical and behavioral health professionals, and for good reason Since its development in the 1960s, the SOAP framework has been useful enough for



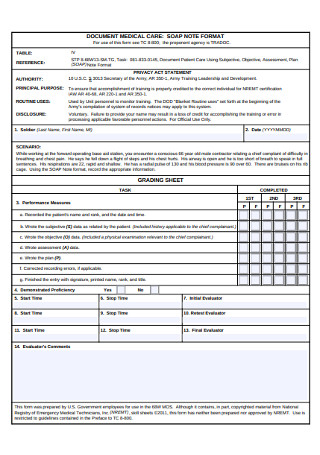
Patient Soap Note Charting Procedures



Soap Notes Sample Medicine Soap A P Surgery Soap Pdf Free Download
What does SOAP abbreviation stand for?Medical Abbreviations Browse thousands of Medical acronyms and abbreviations classified by 38 subcategoriesWhat is a SOAP Note – Definition A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that are used by professionals in the health sector The SOAP note is usually included in the patient's medical record for the purpose of informing




Medical Archives Emottawa Blog




Soap And Detergent Chemistry Uses Properties Facts Britannica
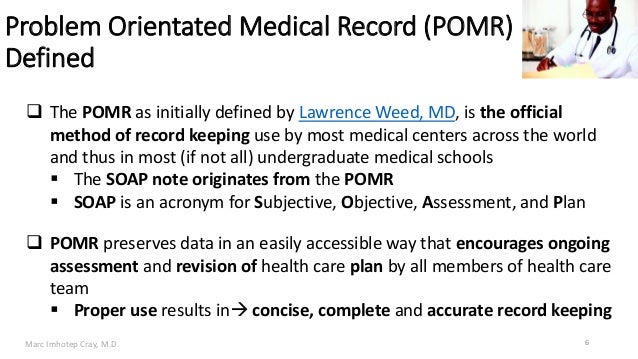
Soap definition is a cleansing and emulsifying agent made usually by action of alkali on fat or fatty acids and consisting essentially of sodium or potassium salts ofIt helps record the patient's current condition and symptoms, past medical records, medication, and other valuable details Primarily, it is a wellstructured document used between practitioners to communicate about a particular patient's medical state The concept was first invented by Doctor Lawrence Weed almost over 50 years backSOAP ( Simple Object Access Protocol) is a message protocol that allows distributed elements of an application to communicate SOAP can be carried over a variety of lowerlevel protocols, including the webrelated Hypertext Transfer Protocol () SOAP defines a header structure that identifies the actions that various SOAP nodes are expected to take on the message, in addition to a payload




Who S Infection Prevention Control Department




Free Soap Notes Templates For Busy Healthcare Professionals
The SOAP Note Template is a documentation method used by medical practitioners to assess a patient's condition It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information It stands for "Subjective Objective Assessment Plan," which provides documentation of a patient's condition, diagnosis and treatment SOAP notes were invented in the 1960s by Dr Lawrence Weed of the University of Vermont and didn't take long to enter widespread use in the medical profession For practical office management purposesMany abbreviations have multiple possible meanings In which part of the SOAP note is medication prescribed?




Handwriting Text Writing Health And Medical Concept Meaning Study And Investigation Of Physical And Mental Wellbeing Canstock



Progress Notes
The term "SOAP" simply refers to the 4 headings in this type of report Subjective, Objective, Assessment and Plan= SOAP The basic rule of a SOAP note is brevity;1 Established procedure to be followed in carrying out a given operation or in a given situation 2 A specific procedure or set of procedures so establishedLooking for online definition of SOAP or what SOAP stands for?




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



Pomr And Soap Notes
Today, the SOAP note – an acronym for Subjective, Objective, Assessment and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share information in a universal, systematic and easy to read format Opening a new medical practice?Pulmonary SOAP Note Medical Transcription Sample Report #7 SUBJECTIVE The patient is here at Dr John Doe's request She has been coughing, short of breath since Friday She said she got it flared up by someone's perfume She was better on Saturday Today, she is worse again, took some DepoMedrol 160 mg today What Does SOS Stand For?



10 Medical Acronyms Eponyms Page 1 Of 2 Medical Chegg Com



Emr Soap Notes Format Cheat Sheet By Deleted Download Free From Cheatography Cheatography Com Cheat Sheets For Every Occasion
What do the abbreviation s o a p mean in medical terms Answers Answer from Kemosdasavage The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission noteThis is not usually a lengthy history detailing all the facts of the patient's health status'Emergency Medical Services' is one option get in to view more @ The Web's largest and most authoritative acronyms and abbreviations resource




Hcm210 Medical Terminology Soap Notes Youtube




What Is Vegetable Glycerine And Is It Keto Perfect Keto




How Soap Notes Paved Way For Modern Medical Documentation




Him 125
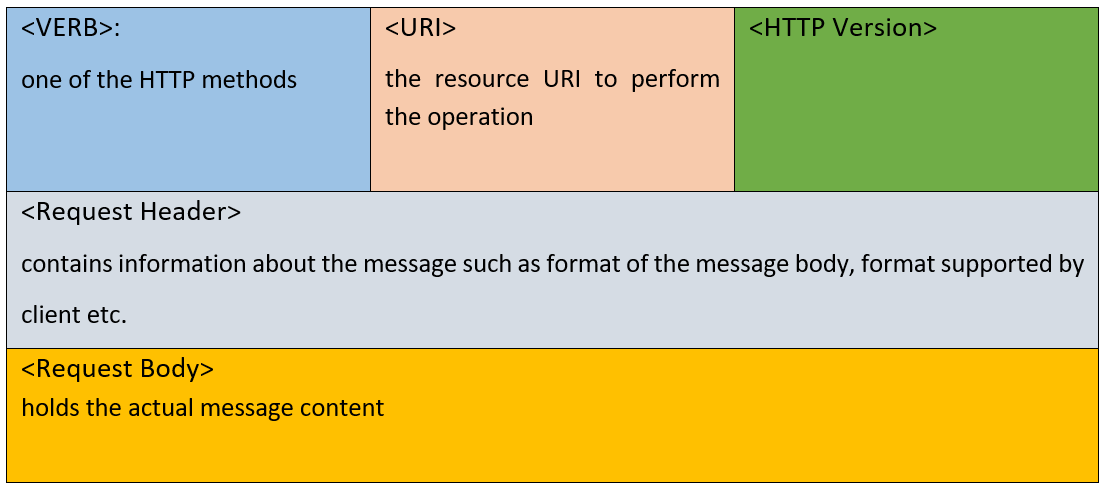



Webservices Soap And Rest A Simple Introduction




Free Soap Notes Templates For Busy Healthcare Professionals



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




What Does Soap Stand For




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
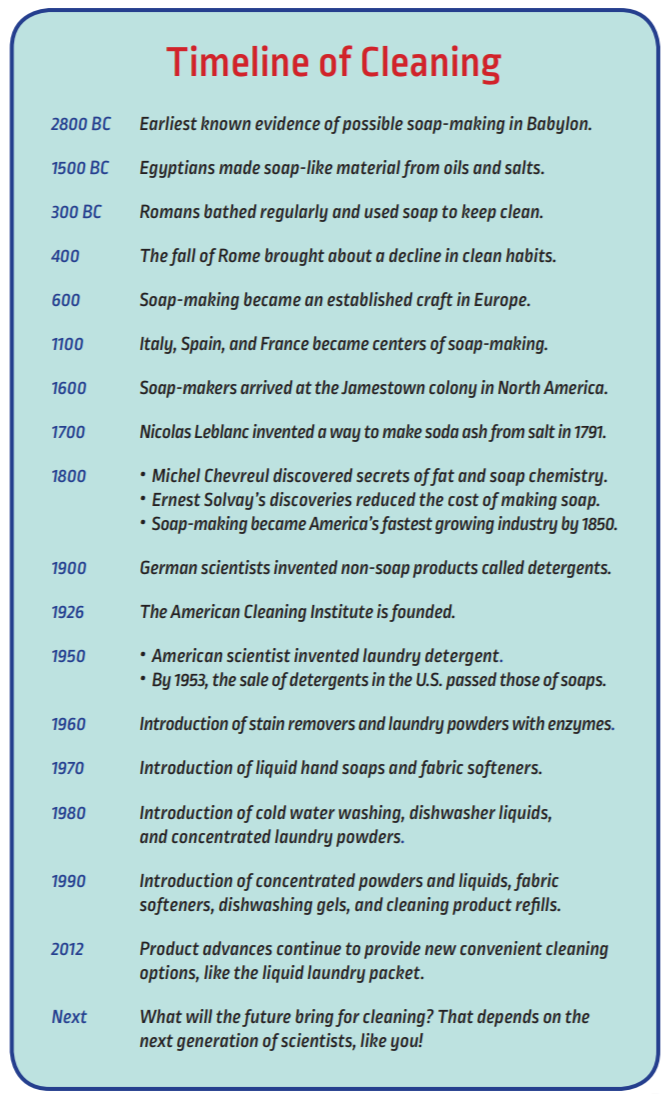



Soaps Detergents History The American Cleaning Institute Aci



1




Infographic S O A P Notes




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




What Does Soap Mean Soap Definitions Abbreviation Finder



1




Tips For Writing Better Mental Health Soap Notes Updated 21



How To Make Soap Notes 7 Steps Instructables




Soap Notes The St John S Pa Program Survival Guide



Soap Subjective Objective Action And Plan Of Treatment By Acronymsandslang Com



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Soap Advertising The Trader As Civiliser And The Scramble For Africa In Imperial Persuaders




The Soap Opera And Its Affect On Media Culture And Society Mr Hughes Ppt Download




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Medical Terminology And Abbrev Pages 1 10 Flip Pdf Download Fliphtml5
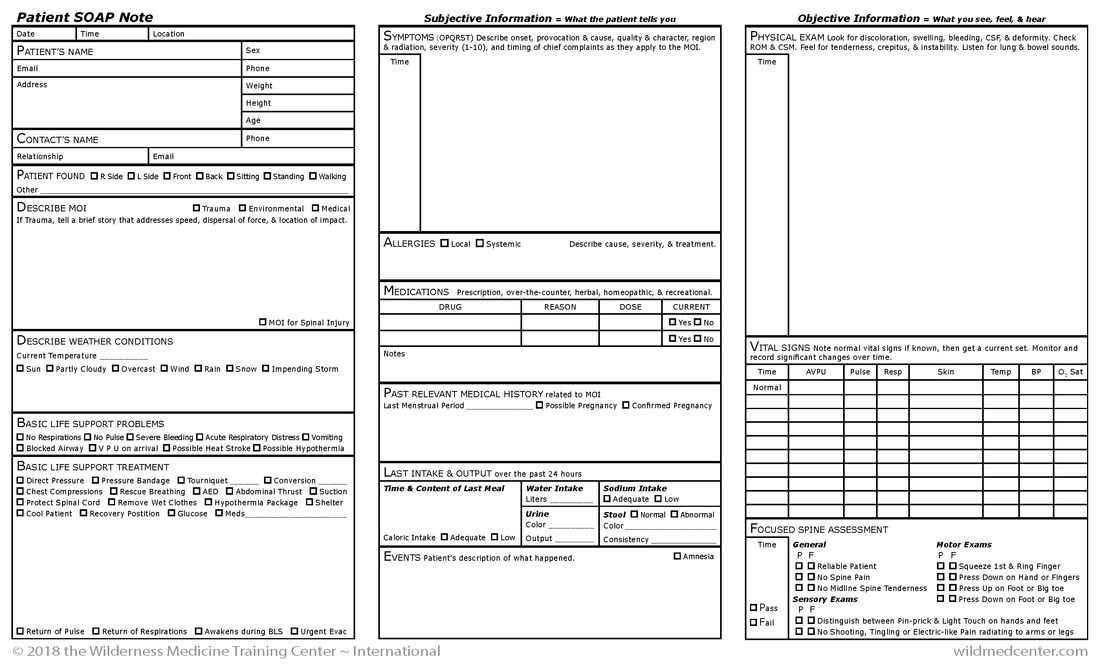



Wilderness Medicine Training Center S Patient Soap Notes
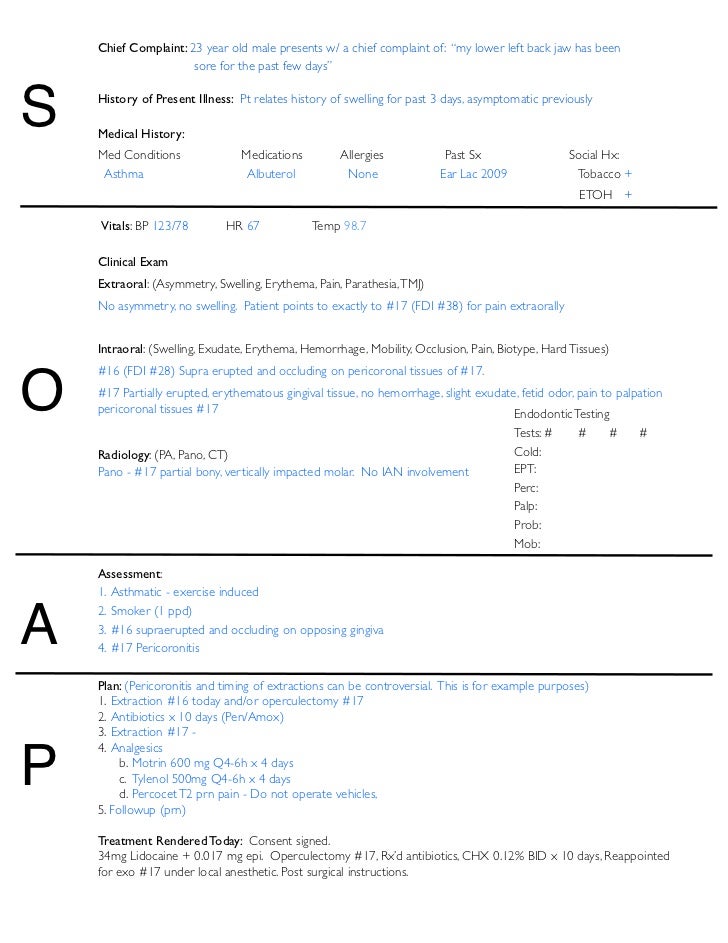



Soap Notes Dentistry Example
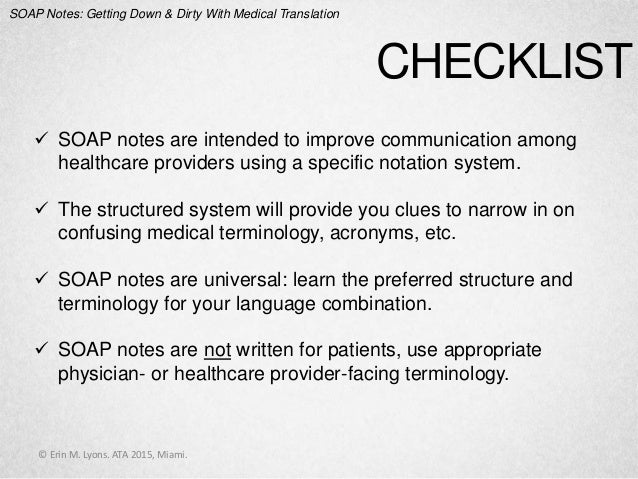



Soap Notes Getting Down And Dirty With Medical Translation




How To Write Incredible Physical Therapist Soap Notes



What Are Soap Notes In Counseling Examples




Soap Notes Flashcards Quizlet




Soap Notes Resources Digital Chalkboard




Soap Notes Youtube



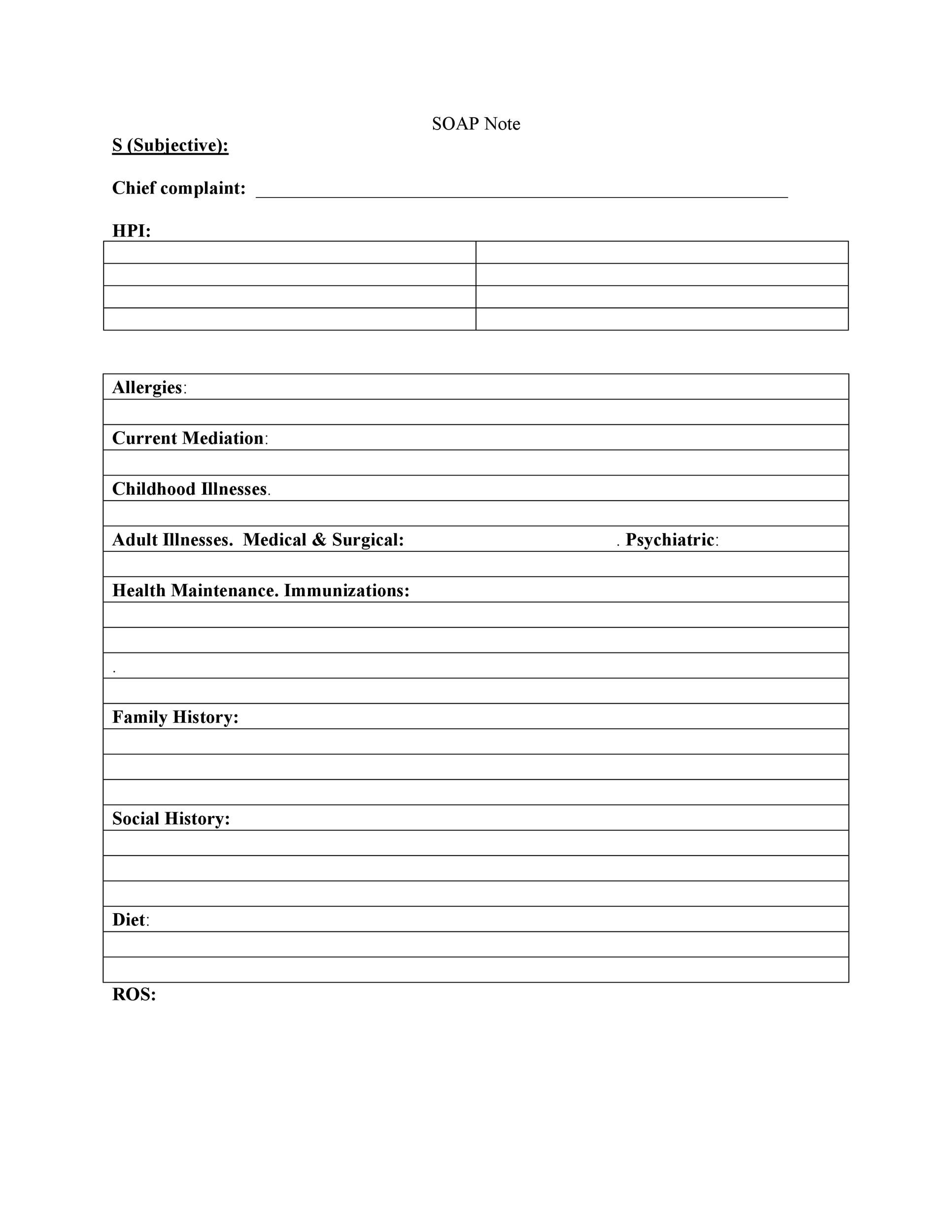
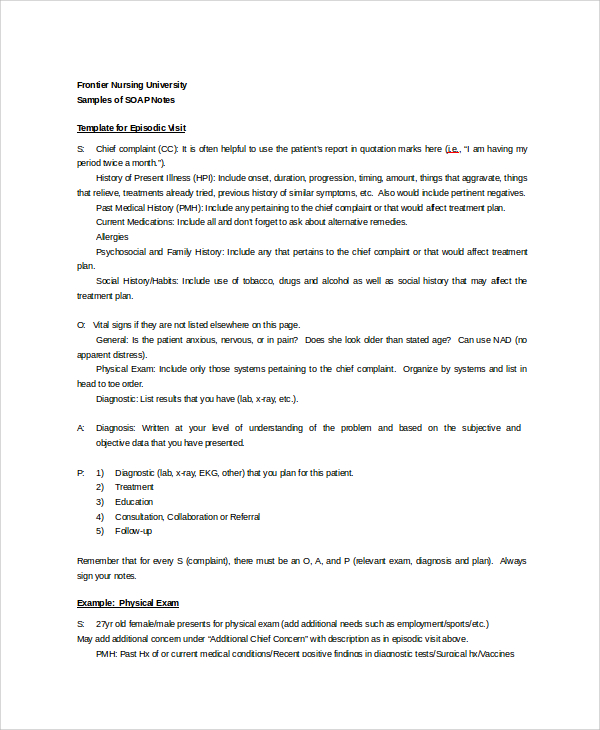
Fcm Unm Edu Education Images Docs Template Clin Soap Note Pdf




Soap Note




How To Write Incredible Physical Therapist Soap Notes




Stay Safe Medical Block Sogam Facebook
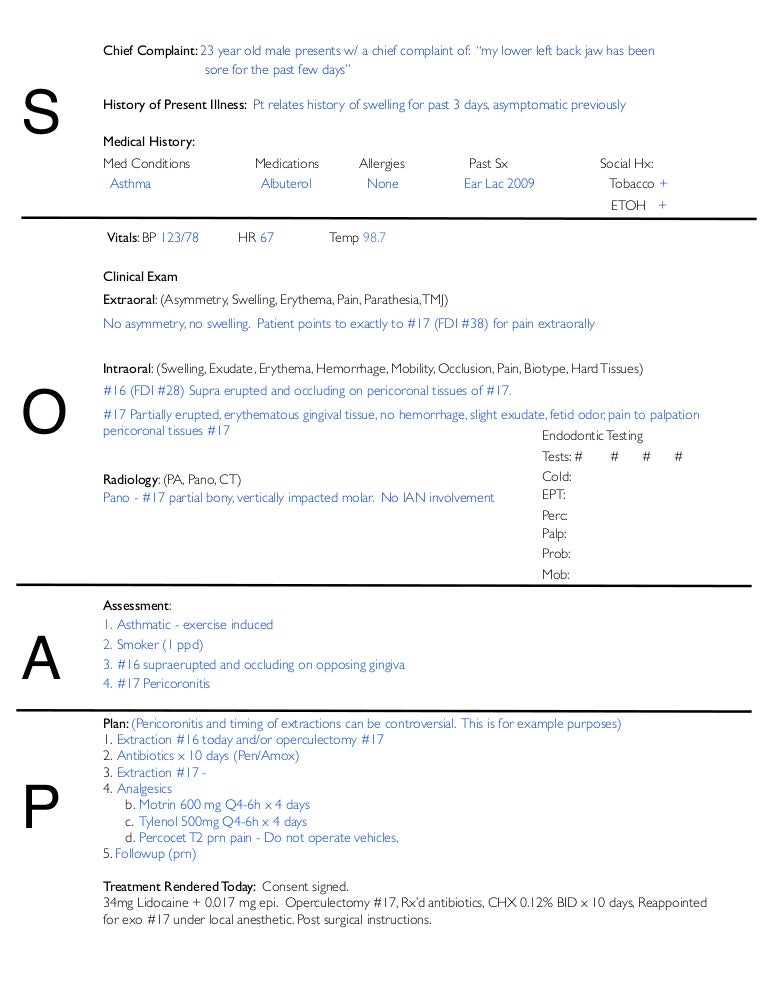



Soap Notes Dentistry Example




Dental Clinic Handbook Revised April 10 Pdf Document




What Are Soap Notes In Counseling Examples
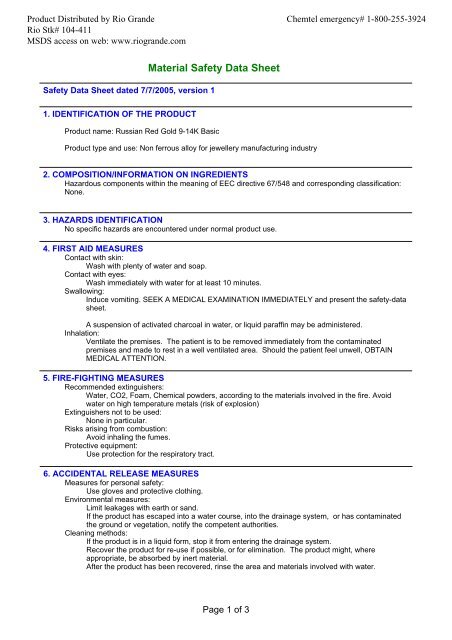



Russian Red Gold 9 14k Basic Msds Rio Grande



40 Fantastic Soap Note Examples Templates ᐅ Templatelab
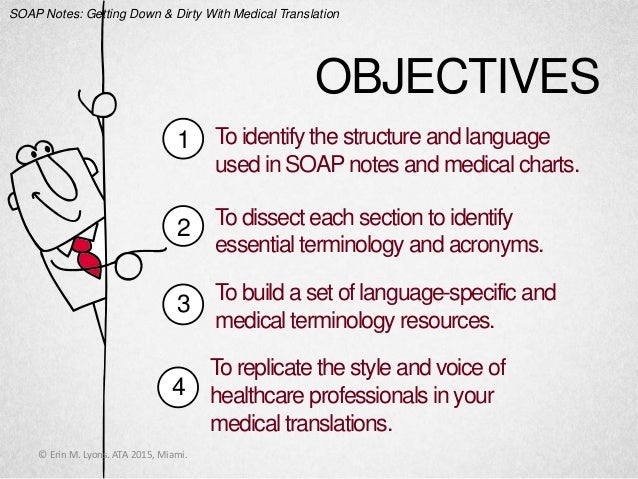



Soap Notes Getting Down And Dirty With Medical Translation



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



What Does S O A P Mean Definition Of S O A P S O A P Stands For Subjective Objective Assessment Plan By Acronymsandslang Com




Hand Washing Wikipedia




How To Write A Soap Note With Pictures Wikihow




Planning Patient Care Health Care Service Delivery



Soap Subjective Objective Assessment Plan By Acronymsandslang Com



Free 15 Soap Note Templates In Pdf Ms Word




No Audio Recording Preparation Ppt Download




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice




Examples Of Soap Notes In Nursing Video Lesson Transcript Study Com



Tips For Writing Better Mental Health Soap Notes Updated 21



Ppt Nutritional Progress Notes Powerpoint Presentation Free Download Id




Blue Rimmed Cold Process Soap Tutorial Soap Queen Recipe In 21 Cold Process Soap Soap Tutorial Easy Soap



Pdf Why We Should Wash Our Hands Of Medical Soaps
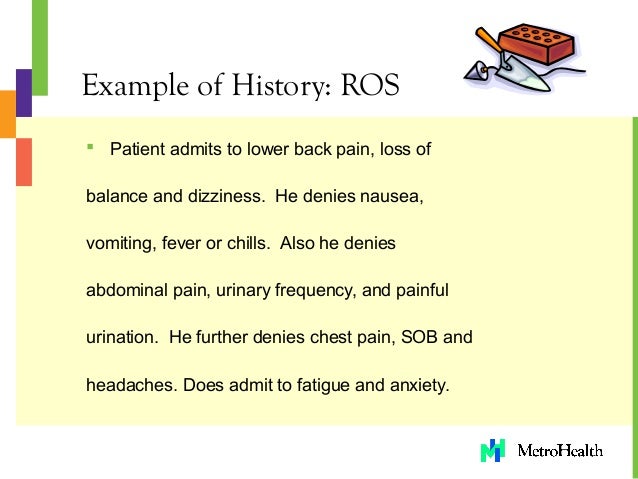



Ros Medical Example
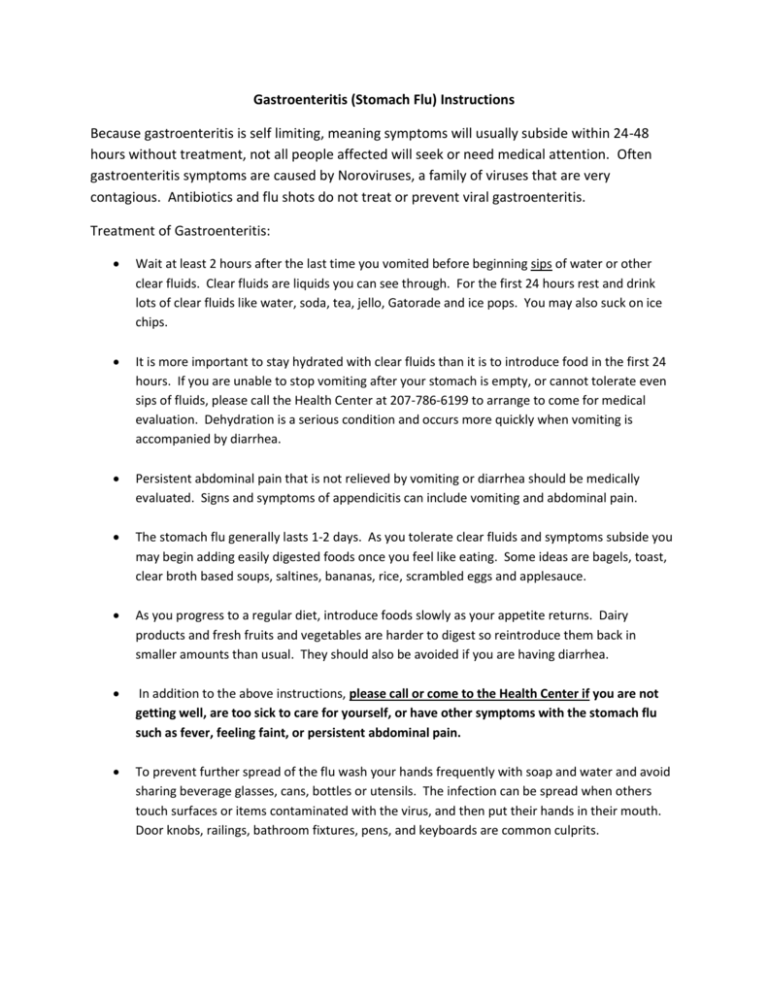



Gastroenteritis Stomach Flu Instructions Because Gastroenteritis Is



Www Lamar Edu Fine Arts Communication Files Documents Speech Hearing Soap Notes Pdf
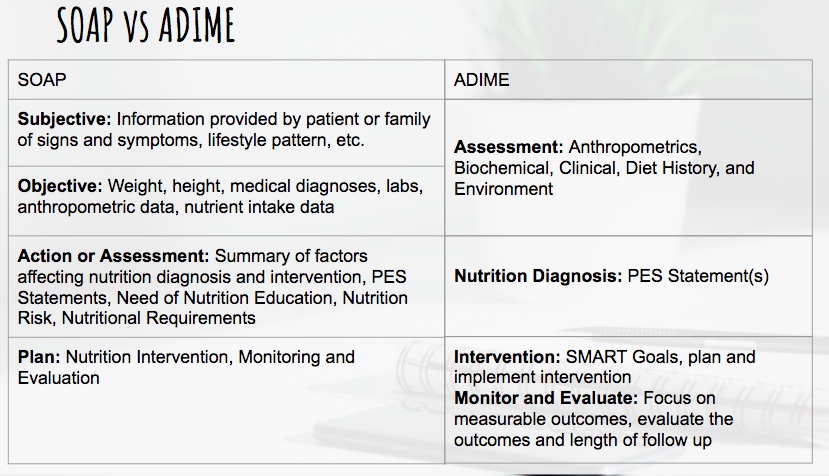



Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




Conceptual Hand Writing Showing Medical Checkup Concept Meaning The Examination Carried Out To Determine The Physical Fitness Primary Medical Precaut Stock Photo Alamy




Free Soap Notes Templates For Busy Healthcare Professionals




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice
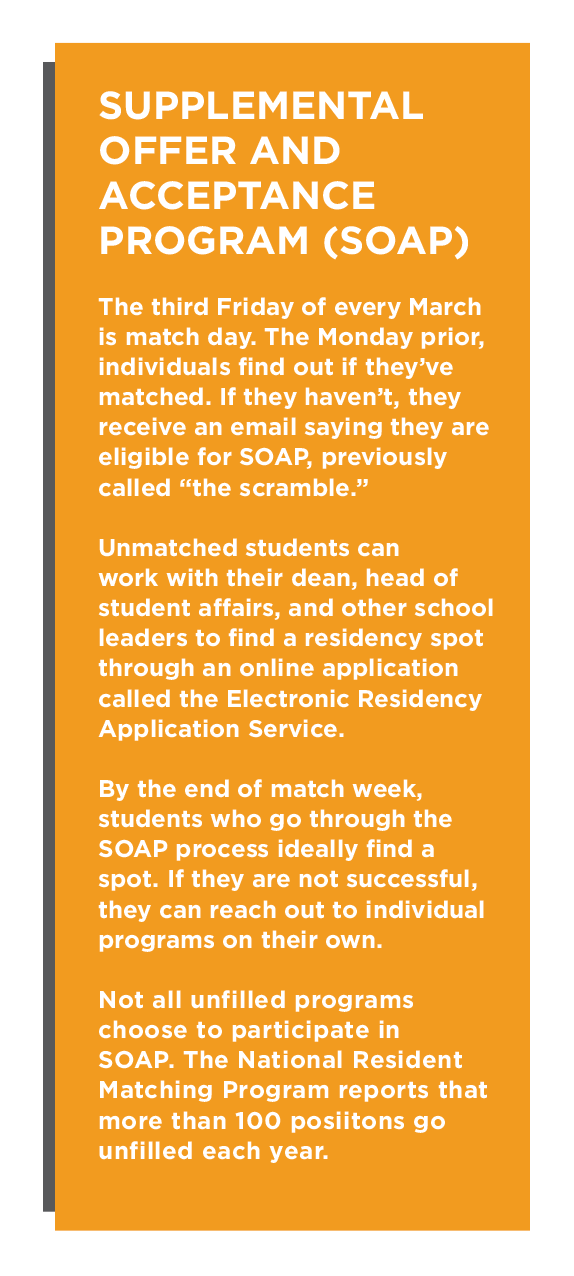



Healthcare Suffers When Medical School Graduates Don T Match Insight Into Diversity




How To Write Massage Therapy Soap Notes Mblexguide



Cuticura Soap Wikiwand



1



1




Soap Note Templates Safetyculture




How To Write Massage Therapy Soap Notes Mblexguide




Say Goodbye To Antibacterial Soaps Why The Fda Is Banning A Household Item Science In The News
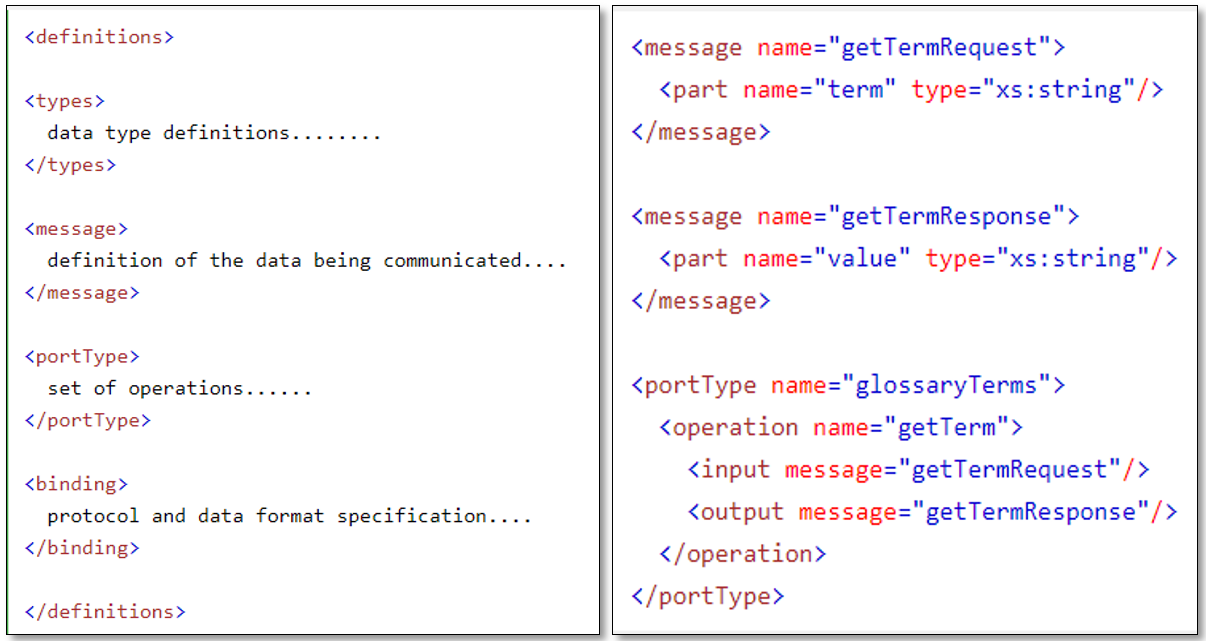



Webservices Soap And Rest A Simple Introduction
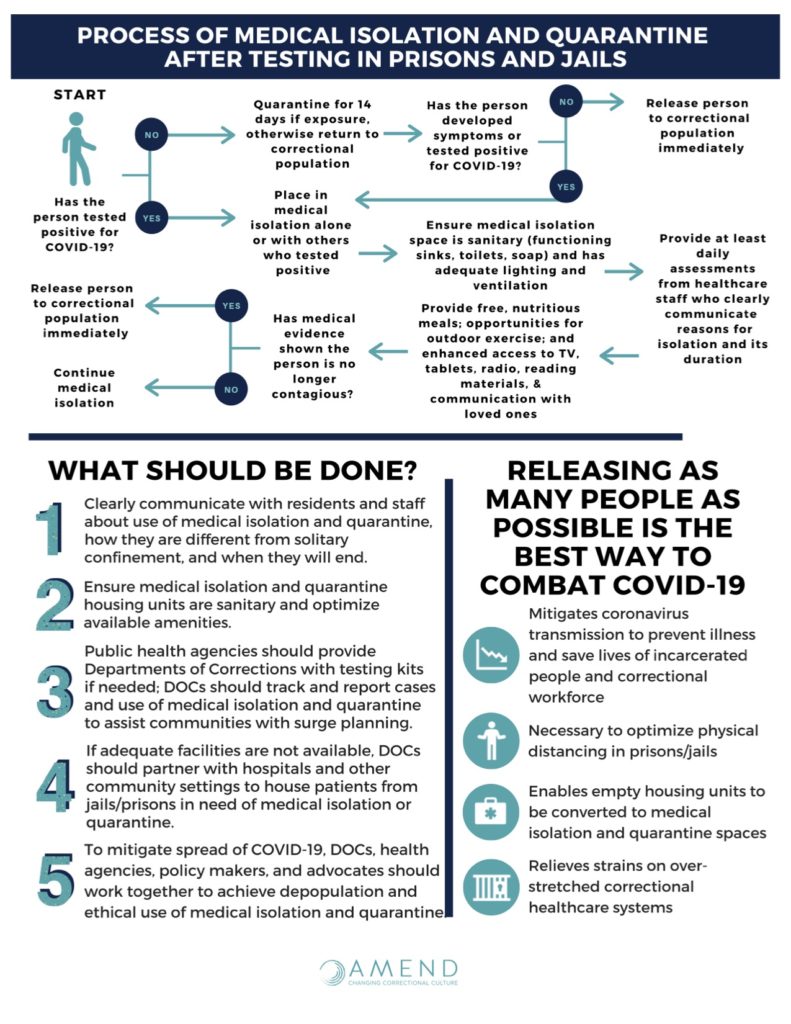



Covid 19 In Correctional Facilities Medical Isolation Amend
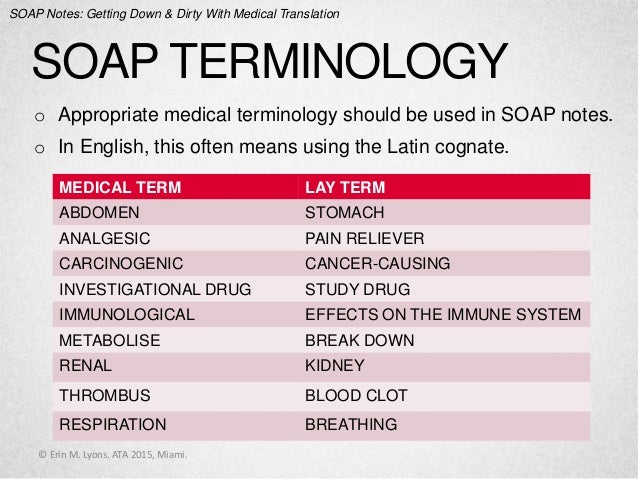



Soap Notes Getting Down And Dirty With Medical Translation



0 件のコメント:
コメントを投稿